Our Care
Focus on MY CARE
We will be unwavering in our commitment to put patients first, involving them in all aspects of their care and providing the most positive experience. Every encounter. No Exceptions.
RVH Supports Those Struggling with Addiction
Previous Stories from 2021-2022 Annual Report
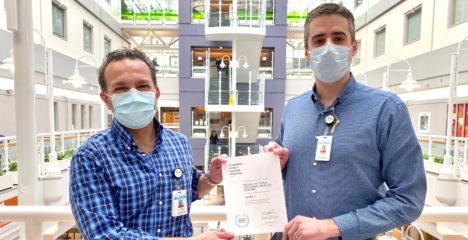
RVH has been recognized as a Level 1 Choosing Wisely Canada hospital. This designation demonstrates the health centre’s commitment to providing exceptional patient care, shortening wait times, and reducing the potential for adverse events.
“This is a significant achievement for RVH and another important step forward in our commitment to safe, high-quality patient care,” says Dr. Ihab Louis, RVH Chief Medical Quality Officer, Deputy Chief of Staff, and Chief of Anesthesia. “Unnecessary testing and treatment is an ongoing issue in healthcare and with patient volumes and wait times ever-increasing, this is a way RVH can help to mitigate that.”
Choosing Wisely Canada is a national organization that promotes and advocates for the reduction of unnecessary tests and treatments in healthcare. Launched in 2014, Choosing Wisely has engaged healthcare professionals to reduce unnecessary tests, treatments and procedures, through tools and resources that make it easier to ‘choose wisely.’
Helpful information and tools which identify tests and treatments commonly used in each specialty that are not supported by evidence and could expose patients to harm, help clinicians “choose wisely”.
RVH will continue to advance towards the Level 2 and Level 3 Choosing Wisely designation in the near future.

With drumsticks in hand, Doug Sutter is ready for his recreation therapy session at Royal Victoria Regional Health Centre.

The 83-year-old Mansfield resident, currently a patient on RVH’s Specialized Seniors Care unit, has recently added DROM to his other therapies, as he works toward improving his health so he can find a placement in a local long-term care home.
DROM is a recreational activity that engages both body and brain. It is the combination of drumming (DR) and mediation (OM). The combination of music and drum rhythms connects the participant to their own inner power through movement using both the right and left hemispheres of the brain.
Using a large ball placed in a container as their drum kit, participants hit the ball with drumsticks fast and slow according to the music being played.
During the class Katherine Lee and Kristy Boyce, Recreation Therapists, who are certified DROM instructors, lead the small group of patients through opening warm-up stretches to full on drumming.

“It’s movement that is fun and easy,” says Lee. “It is a process that utilizes functional intervention, education and recreation participation to enable people with physical, cognitive, emotional or social limitations to achieve or maintain skills, knowledge and behaviours that will allow them to enjoy their leisure optimally and function independently.”
The benefits of DROM include reduced fatigue, hostility, depression and other burnout symptoms. The practice incorporates specifically designed beats to help reduce anxiety and stress, promote positive feelings and improve focus and concentration.
“Patients move at their own pace, listening to their own body, knowing that there is no right or wrong way to do it. This therapy is great for anyone as it improves range of motion and it’s pretty good cardio,” says Boyce. “The 30-minute class typically starts with a focus on breaking and a warmup, followed by three components of cardio, stretching and then free moment and cool down. We encourage patients to participate in free moment and to even lead the class as is provides a sense of belonging.”
DROM is just one of many activities that stimulate both brain and body available to patients on this unit. Some others include bowling, creative arts, trivia, armchair yoga, walking groups and church services with the Spiritual Care team all with the focus on providing patients with the best experience possible.
While all these activities help to improve a patient`s quality of life, it is the loud DROM class that certainly attracts the most attention, as nurses and other patients frequently stop to watch through the large windows of the therapy room.
And there is no doubt the star of the show is Sutter. When he first arrived at RVH he couldn’t walk. In and out of RVH for months, recreation therapy has helped him so much that he is now able to get around using a walker. On this day though, he’s a drummer in a rock band keeping up to the beat of the song Footloose.
“I’m trying to participate in as much activity here at RVH that I can,” says Sutter. “This class is exercise, but I also enjoy the camaraderie. You get to know the other patients and get to talk to them. You know, when I came in here, I couldn’t even walk.”
And Lee sees only further progress in his future. “This class is setting him up for success in his next placement.”
Ideally, that success will be in a local long-term care home, unless of course Tommy Lee or Phil Collins needs a backup drummer.

 When Erika Gilbert got the news that her beloved grandmother’s health was declining rapidly, she was desperate to see her one last time.
When Erika Gilbert got the news that her beloved grandmother’s health was declining rapidly, she was desperate to see her one last time.
Unfortunately, the safety protocols RVH was forced to introduce to protect patients and staff during the pandemic prevented her from visiting the health centre. So, she turned to RVH’s Patient and Family Experience team for help.
At RVH, the patient experience (measured monthly) is paramount, and family support is a key component of a patient’s care. TEAM RVH works hard to balance the need for family connection with necessary safety requirements.
“RVH has made it our mission to provide exceptional patient care and we understand family support is vital to a patient’s wellbeing and recovery,” says Janice Skot, RVH President and CEO. “Visitor restrictions have been necessary to keep patients safe during the pandemic, but we recognize how difficult it has been for, both, patients and their families.”
By continuing to focus on patients and their families and doing everything possible to ease their fear, anxiety and loneliness, RVH saw no decline in patient satisfaction during the pandemic. In fact, the health centre maintained excellent monthly scores ranging from 73 to 79 per cent, well above RVH’s targets and the provincial average of 70 per cent.
In the absence of in-person visitation, RVH made virtual contact through iPads an integral part of patient experience and assessment during the pandemic. When leaders rounded on patients, family members were encouraged to take part on videos calls to support the patient and partner in decision-making process.
At each shift change, nurses included patients and their virtually present family members in the bedside handover. In the Neonatal Intensive Care Unit, nurses used FaceTime to share babies’ care and milestones with anxious parents.
Even the Blue Brigade, RVH’s celebrated volunteer team, which hasn’t been in the the health centre since the pandemic began, resumed patient visits through virtual means.
In addition, a Visitor Appeal Committee was created to review visitation requests from patients and families that fell outside the official policy, like Erika’s. The Patient and Family Experience team quickly forwarded her request to the committee which granted it. Erica was able to say good-bye to her grandmother in-person before she passed away the next day.
“There was a moment when I asked her if she knew who I was,” says Erika. “Even with all of my personal protective equipment on she said, ‘You’re Erika and I love you so much. It means the world to me that you’re here’ and she squeezed my hand. These are words I will never forget and that I might not have heard without the Patient Experience team. I can’t thank them enough for their compassion, care and support.”

Recovery from orthopedic or total joint replacement surgery is no walk in the park.
Outside the actual procedure, pre-op preparation and post-op care involve so many details and expectations that, prior to COVID, patients had to attend education classes at RVH to learn them all. When the pandemic made in-person meeting impossible, the Surgery team pivoted to deliver virtual support to patients until things could return to normal.
Two years later, this “temporary” virtual care model has become the new normal.
Recently, Ontario Health offered a one-time funding grant designed to help health centres increase access to care for patients through virtual programs and services, transforming how they support integrated care delivery now and in the future.
The Surgery program elected to use their grant to improve and expand on its virtual care model through Seamless MD, a customized app designed specifically for RVH total joint replacement ortho patients.
SeamlessMD can be accessed on any smartphone, tablet or computer. The app helps patients prepare for surgery and guides them through post-op care. It offers virtual check-ins before the procedure, day of surgery and post-op to identify medical concerns and track medication and pain management. The app monitors side effects to help catch complications sooner and therefore improve overall patient outcomes, and features automated self-management recommendations based on patient self-reported symptoms with personalized education. The app also allows a caregiver to be enrolled to assist in the patient’s journey.
Patients began using the app in February and their feedback has been overwhelmingly positive.
“It gave me confidence that I was on track with my aftercare,” one patient remarks. “It also made me feel that it was okay to still have pain and to take things one step at a time.”
Another said, “I felt more comfortable doing the required exercises. Also, it’s far easier to get rest without the distractions of hospital life around you!”
The app is not mandatory. Patients not wanting to use it receive the necessary information in a hard copy patient handbook. But the app has proven that a virtual experience can be just as supportive and informative as an in-person one.
As another patient said “With the app I didn’t feel so alone. Being completely ignorant about medical things, it really felt like someone was here helping me.”